|
Presbyopia is a natural process that typically occurs in the 40’s and reduces ones ability to read when vision is corrected for distance. This problem is a frustrating one, especially for those who enjoy contact lenses. When contacts are used to correct far away vision in someone who is presbyopic, additional options are needed to allow comfortable reading. Over-the-counter reading glasses and mono vision are two options that offer both advantages and compromise. Multifocal contacts continue to improve in viability but typical “one-size-fits-all” lenses don’t offer options for patients with astigmatism. It is important to remember that, unlike bifocal or progressive glasses where distance and near vision can be put in different parts of the lens, contact lenses are stable on the eye and all powers must be contained in a small pupil-sized region, making the task of crisp vision at all distances much more difficult. Here we will discuss options for patients with astigmatism who need distance and near correction and desire binocular vision free from reading glasses:
Custom soft multifocal toric lenses Unlike one-size-fits all soft contact lenses, custom soft lenses are made based on a patients corneal parameters including diameter, curvature and eccentricity (rate of flattening). Not only is the fit customized to improve comfort, the optics are also made to specifically match the patients prescription. These lenses are made-to-order and therefore all specifications are customizable, even the material the lens is made from.
1 Comment
Imagine never squinting and shielding your eyes from blinding sunlight, or feeling the strain of eight-plus hours under fluorescent bulbs. That’s the allure of Acuvue’s anticipated line of light-sensitive, vision-correcting contact lenses, Acuvue Oasys with Transitions. Each contains a filter that senses the amount of light entering your eye and automatically darkens or lightens to maximize comfort. The contacts, which have been in the works for over a decade, received FDA clearance in 2018. They were also voted one of TIME Magazine's Best New Inventions in 2018. Here's why. ACUVUE® OASYS with Transitions is a first-of-its-kind contact lens for contact lens wearers. These lenses combine a proven ACUVUE® OASYS (senofilcon A) material with Transitions™ Light Intelligent Technology™. The result is a lens that seamlessly adapts to changing light, providing all-day, soothing vision.
When asked about experiencing moments when bothered by light, 64% of consumers admit to being bothered by bright light daily. 94% of those who reported they were bothered by bright light daily use compensating behaviors (such as eye shading, squinting, turning off lights and turning down screen brightness) to manage it. ACUVUE® OASYS with Transitions™ activates in less than a minute and quickly fades from dark to clear when going from outdoors to indoors. At Kirkwood Eye Associates, we are proud to be one of the first practices in the Saint Louis region selected to carry this revolutionary new contact lens. To make an appointment or to learn more information call, 314.394.3045.
The fact is, nearly 90% (and more by some estimates) of dry eye syndromes can be traced back to eyelid disease. Our lids contain so many structures that are vital for producing and maintaining a healthy ocular surface environment including accessory lacrimal (tear) glands, meibomian (oil) glands, the lid wiper structure and more. If any of these structures are inflamed or obstructed, they won’t work properly and this results in a breakdown of the complex structure of the pre-corneal tear film. What are some of the causes of lid disease?
Demodex Blepharitis: This condition is caused by an over-infestation of the demodex mite in and around our eyelash follicles. Everyone has demodex mites, but some people have an over-colonization on their eyelids. This, in my opinion, is the single most common cause of dry eye syndrome because it results in inflammation, reduced basal tear production and meibomian gland dysfunction. These patients are often mis-diagnosed as having an autoimmune condition or ocular rosacea. Ocular Rosacea: It is my experience that almost all ocular rosacea patients suffer from demodex blepharitis. In fact, there is strong evidence that rosacea in all forms is strongly linked to the demodex mite. Rarely, patients can show red and inflamed eyelid margins with no form of infestation, but this is definitely the exception to the rule. Bacterial Blepharitis: We all have trillions of bacteria that live on us and inside of us, referred to as our normal flora. Sometimes, a few too many of these organisms accumulate along the eyelashes. The eyelashes offer protection, moisture and oils that all combine to promote microbial growth, making bacterial blepharitis a common culprit of dry eye. The bacteria promote inflammation, thereby reducing gland function. They also produce exotoxins and lipase that disrupt our tear film and ocular surface. This condition can be difficult to treat with traditional therapies because the bacteria will form biofilms along the lid margin, protecting them from soaps and other treatments. These biofilms also clog tear and oil glands on the lids. Meibomian Gland Dysfunction: The meibomian glands line our eyelids and secrete an oil (lipid) layer that coats and protects our tears. This lipid layer is solely responsible for the stability and even distribution of tears across the ocular surface and also prevents the tears from evaporating between blinks. Almost all dry eye has some component of meibomian gland dysfunction. These glands can become clogged for a number of reasons including genetics and all of the conditions listed above. Extended electronic device use (and the subsequent lack of blinking) is the main cause for the steep rise in this condition in recent years. Once these gland become significantly clogged, they must be opened through in-office procedures. What Can Be Done? The first step is getting a proper diagnosis by your eye doctor who specializes in dry eye and lid disease. Testing for dry eye includes meibomian gland imaging, digital tear film analysis, vital dye corneal staining analysis, blink analysis, tear film osmolarity testing and ocular surface and eyelid examination. We often epilate (pluck) an eyelash for microscopic examination in the exam room. There are a variety of at-home treatment options including prescription drops, eyelid cleaners and heat therapy, but most patients fail to find sufficient relief with these products and exercises. For the majority of cases, we start with tailored in-office treatments to remove the offending cause of the lid disease and treat the clogged glands. There are a variety of procedures that can target demodex mites, bacterial blepharitis, eyelid margin inflammation, meibomian gland obstructions, bacterial biofilm and more. From there, we send the patient home with maintenance therapy products to enhance the in-office treatments. Most of these procedures are brand new and not covered by medical or vision insurance. However, the cost is typically less than the cost of over-the-counter and prescription eyedrops when extrapolated over time… and are far more effective! The goal of modern dry eye therapy is to greatly reduce or remove the need for eye drops during the day. Next time you feel any one of the common symptoms of dry eye (variable vision that changes with the blink, itching, burning, excessive tearing, redness, tired or heavy eyes, reduced contact lens wear time), look at your eyelids! They’re usually the ones to blame. An annual eye exam is about more than just updating your prescription for contacts or glasses. While this is important to ensure you're seeing to the best of your ability, there are other reasons a visit is crucial at least twice a year. A routine eye exam can detect other serious health problems before you're even experiencing symptoms. Did you know that many people first learn they have serious health conditions like brain tumors, high cholesterol, diabetes, high blood pressure, and even cancer from a routine eye exam?
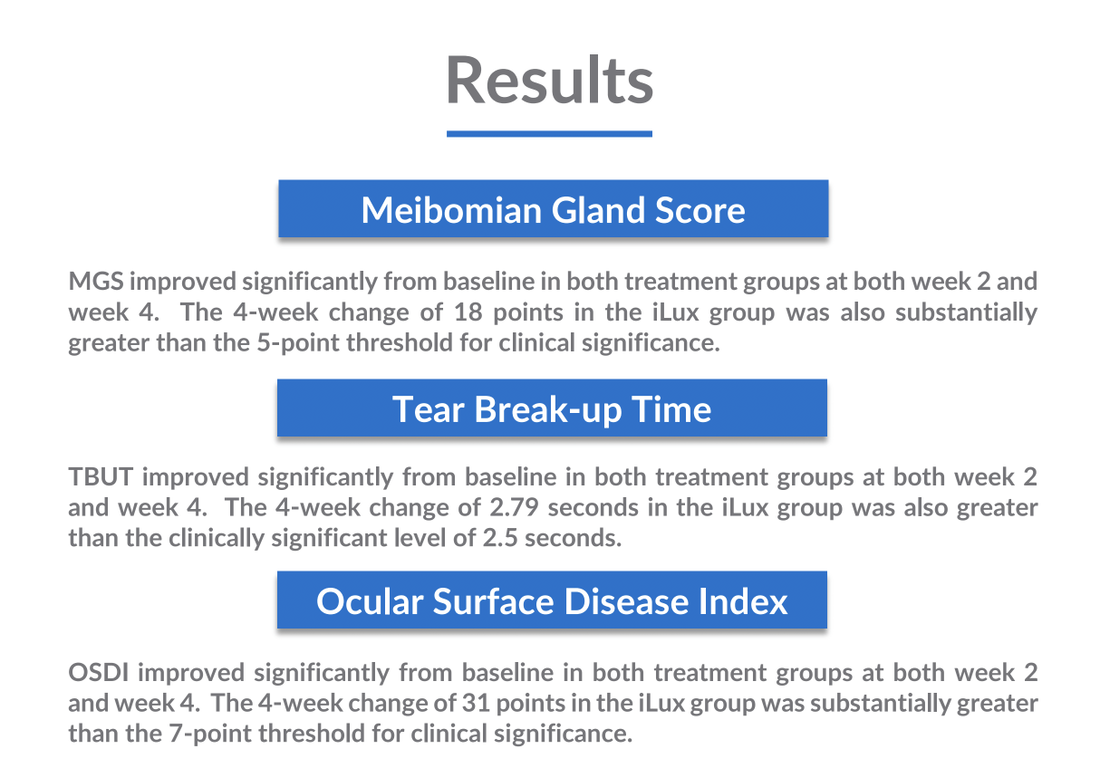
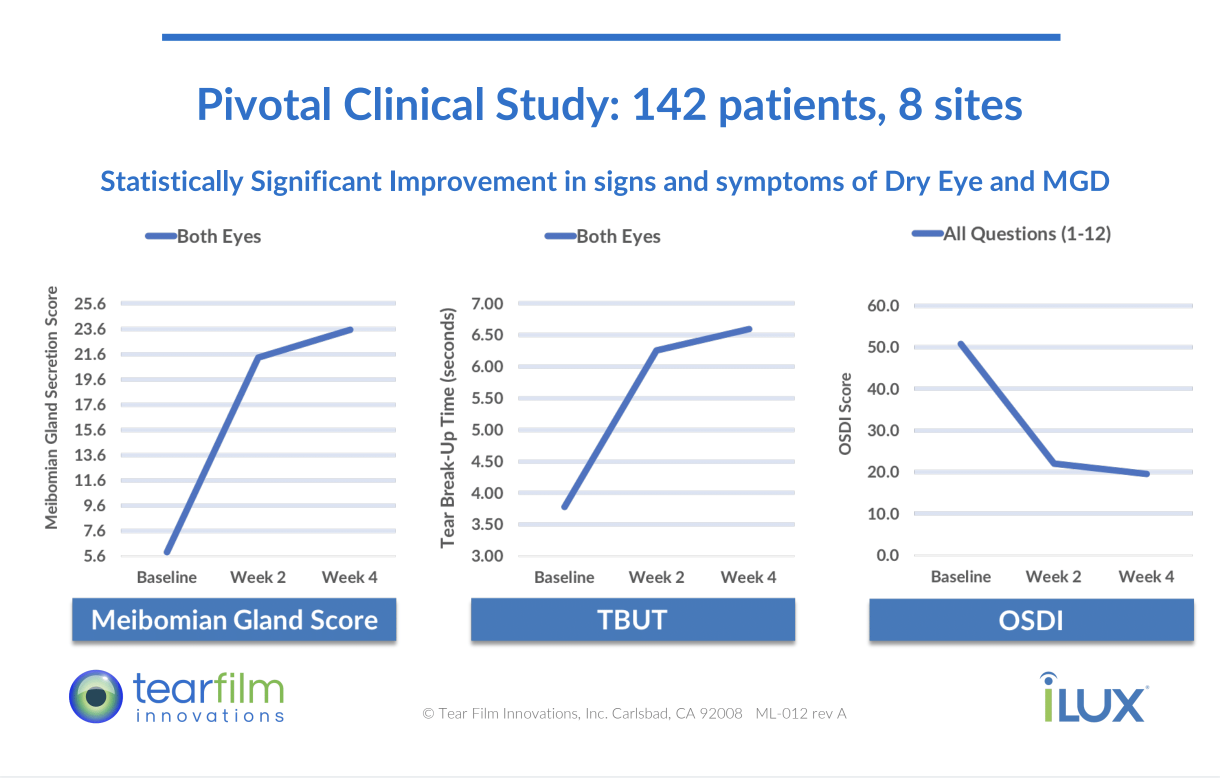
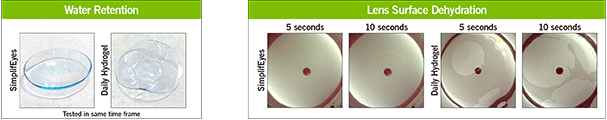
Our eyes are a very effective window to our overall health. During a comprehensive eye exam, your doctor can observe and evaluate the health and condition of the blood vessels in your retina. These are a good predictor of the health of the blood vessels throughout your body. Conditions such as diabetes, hypertension and hypercholesterolemia all are visible by changes in the appearance of the retinal blood supply and blood vessels. Your doctor will also look for eye muscle imbalance, vision disorder, and eye disease that could potentially cause future problems. Many people wait until they notice a change in their vision to see a doctor. But eye problems are often silent - meaning they have no symptoms, which can be dangerous if you are waiting to see a change before making an appointment. Annual eye exams are especially important for anyone with diabetes or who might be at risk for the disease (due to obesity, family history, etc). More than 30 million Americans with diabetes and another 84 million are at risk for developing diabetic eye disease which is a leading cause of blindness among adults. In its early stages, diabetic eye disease has zero visible symptoms; only a comprehensive eye exam can detect signs of the disease. The sooner treatment is sought, the likelier the vision can be preserved. If no treatment is given, vision loss will ensue. So you've had a vision screening? It's not the same as a complete exam. Screenings are partial, limited eye evaluations that take place outside an eye doctor's office. While they can be helpful in detecting some problems with vision, it is a limited exam. At your optometrist's office, a thorough eye exam takes deeper look at your vision and how it affects your overall health. Eye history and family history are also considered as a preventative measure to stop eye disease before it begins. What are you waiting for? Don't put it off any longer. Even if you think you have perfect vision, an annual eye exam can be one of the best things you can do to protect your overall health and wellness. Start the new year right with a visit to Kirkwood Eye Associates. We are excited to be the first practice in the St. Louis area to offer the iLux Dry Eye Treatment System. The iLux treats meibomian gland dysfunction (MGD), the leading cause of dry eye disease. Patients with MGD are unable to properly produce and sustain the vital lipid layer of the tear film, resulting in variable blurred vision, eye strain, irritation and tearing. This occurs when the oil-producing meibomian glands in the eyelids quit working properly, resulting in solidified and unhealthy oils being released onto the surface of the eye. The most common cause of MGD is extended near work (i.e. computer, tablet, smartphone). The iLux device targets the oil-producing meibomian glands in the eyelids. It uses heat and compression to unblock the glands and clear thickened and unhealthy meibum, allowing the production of clear and healthy secretions that stabilize the tear film and result in improved vision and comfort. The treatment takes about 10-15 minutes and can be done in the exam chair. It is not covered by insurance and costs $335 total for both eyes. Results can last up to a year but some find it beneficial to repeat 6 months after the initial treatment. Some patients notice symptom improvement immediately, but improvement can continue for up to 4 weeks as the new oils refill the glands. Please see the FDA study results and information video below and feel free to call us with any questions. Here at Kirkwood Eye Associates we are proud to announce that we are the first practice in St. Louis to receive the new SimplifEyes daily disposable, soft contact lenses by SynergEyes. This revolutionary soft lens is the first of its kind and promises superior vision and comfort thanks to the inclusion of Tangible molecules imbedded in the contact lens matrix.
Contact lens dryness and discomfort is the number one reason for contact lens drop out. Soft lenses “steal” our tears in order to keep their shape, making patients with even the mildest dry eyes symptomatic at the end of the day. Tangible molecules effectively bind water molecules and retain them within the lens matrix for much longer than standard soft contact lens materials. This allows for all day comfort and visual stability, even in those who have failed other types of soft contact lenses due to discomfort. As a specialty contact lens practice, we have used Tangible coatings with tremendous success on rigid gas permeable lenses since the technology was introduced two years ago. This is the first soft contact lens product to incorporate this revolutionary molecule. Currently, SimplifEyes lenses are only available to treat near sightedness (up tp -6.00) and far sightedness (up to +4.00). They do not offer powers to correct astigmatism, though this could be an option in the near future. The lenses are “single-use” and should be disposed of after one day of wear. They are not approved for overnight wear. They are priced less than other premium daily disposable lenses. If you are a current Kirkwood Eye Associates contact lens patient who has been seen for a contact lens evaluation within 12 months and you are interested in trying SimplifEyes lenses, contact our office for a free 5 day trial pack (if your prescription is within the current available parameters). If you are not a patient or have not had a contact lens evaluation in the past 12 months, call for a fitting today and receive your free trial. Please contact our office with any questions. Dry Eye Disease is a chronic condition that affects millions of Americans. The disease exists along a spectrum that starts at mild (often asymptomatic) to severe and debilitating. At Kirkwood Eye Associates, we follow a progression in treatment options to meet the need of any dry eye patient. While dry eye is not curable and in many cases requires life-long treatment, it can be controlled effectively.
Mild/Moderate dry eye can manifest with no symptoms at all, or can cause mild symptoms of blurred vision, itching, redness, tearing, and grittiness. When we see this stage, we first must determine the type of dry eye and whether the symptoms are caused by the tear glands (the main lacrimal gland and accessory lacrimal glands) or the eyelid oil glands (the meibomian glands). While eyelid glands are more often to blame, it’s typically a combination of the two systems. Initial treatments include warm compresses, omega 3 supplements, lid cleansers and tear supplements (artificial tears). Severe dry eye can range from the constant need of drops or other supportive therapy, to severe pain and depression. Treatment options here are plentiful, mainly because there is no perfect treatment. Which treatment is best for an individual patient depends on a multitude of factors. Here is a list of dry eye therapies offered at Kirkwood Eye Associates: Medical Therapy: Prescription eye drops including corticosteroids, Restasis and Xiidra are commonly used to reduce inflammation and improve the ocular surface environment, allowing some patients to produce more tears. Punctal Occlusion: The watery part of our tears is secreted onto the surface of the eye from the lacrimal gland and then drains off of the eye through the puncta (one on the upper and one on the lower lid near the nose) into the nasal cavity. Punctal plugs are small, painless devices that slow the drainage of tears off of the surface of the eye. This allows your own natural tears to stay on the eye longer, reducing surface dryness. LipiFlow: This unique in office procedure utilizes a device that is placed on the eyes and uses a combination of heat and pressure to clean out the meibomian glands that are crucial for producing the oil layer of our tear film. This oil layer protects the tears from evaporating and helps distribute them evenly over the surface. Chronic inflammation can cause these glands to clog, eventually leading to gland atrophy (death), making regular expression extremely important to the long term health of the eye. Serum Tears: A newer technique gaining popularity is the utilization of your own blood serum as a healing agent for the ocular surface. This process involves drawing blood and spinning it down to a serum that is put in drop bottles. They are then used as eye drops to promote comfort and healing of the ocular surface Scleral Shell: This technique is reserved for individuals with severe tear deficiencies, but it can be highly effective and life changing. A scleral shell is a large rigid contact lens that fits over the cornea, trapping behind it a layer of hydrating saline. Comfortable and easy to wear, these devices bathe the cornea in hydration, alleviating the symptoms of dry eye throughout the day. The also have an added benefit of vision correction, as they can be powered to allow you to see without the need for glasses.
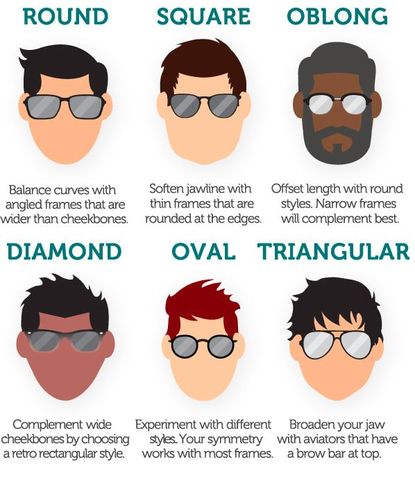
#10. CONTACT LENSES ARE UNCOMFORTABLE
Designed to be as comfortable and non-intrusive as possible, modern contact lenses are barely noticeable. Early iterations of contact lenses could be uncomfortable for some wearers because they were made of glass or hard plastic. They're now made of high-tech materials such as silicone hydrogel. With these materials, oxygen is able to enter the eye easier, nourishing the cornea and so that users often don’t even notice them. #9. CONTACT LENSES ARE A HASSLE Wrong! One-bottle contact lens care systems make cleaning and disinfecting your contacts simple. You can also choose to eliminate contact lens care altogether by wearing daily disposables or 30-day extended wear contact lenses. #8. ASTIGMATISM MEANS I CAN'T WEAR CONTACT LENSES Modern contact lenses have come along way over the years. We are now able to cater to many different eye conditions, including astigmatism. This can actually be corrected by a wide range of toric contact lenses. Even better... astigmatism prescriptions are available for daily disposable, extended wear and monthly lenses. #7. I'M TOO OLD TO WEAR CONTACT LENSES Says who?There is no set age limit as to how old you can be to wear contact lenses. Contacts now come with the option of varifocal and bifocal. This means that older eyes can wear lenses, regardless of whether they require prescriptions for distance and/or reading. #6. I'M TOO YOUNG TO WEAR CONTACT LENSES Similarly to the lack of an age limit on contact lenses, there is no universal age regarding when you can start wearing them. Prescribing contacts is at your own parental discretion. The maturity and capabilities of the child should be considered when deciding whether contacts are suitable for your child. Fortunately, contact lenses are very easy to maintain. Daily disposable lenses require no special storage or cleaning, making them perfect for our younger patients. #5. CONTACT LENSES ARE TOO EXPENSIVE Simply not true. Contact lenses can sometimes be less expensive than a good pair of eyeglasses. Even daily disposable contact lenses, once considered a luxury, can cost only about a dollar a day. #4. CONTACT LENSES FALL OUT EASILY Older contact lenses were composed of rigid materials, making it easy for them to pop out of the eye during intensive activities like sports. Rigid materials also had the potential danger of damaging the eye in the event of blunt trauma. Modern lenses are designed to fit much more closely to the natural contour of the eye. This means it is very rare for them to pop off of the eye, making contact lenses a convenient option for vision correction in sports. #3. I WILL NEVER BE ABLE TO GET THEM IN MY EYES Of course you will! It might seem difficult at first, but our team of eye care professionals will make sure you learn how to apply and remove your contacts before you leave the practice. Most people become adept at handling contact lenses much faster than they anticipate! #2. CONTACT LENSES CAN GET STUCK BEHIND MY EYE FALSE. Simply put, it is not possible for contact lenses to get stuck behind your eye. The Conjunctiva lines the inner eyelids, folding back on itself to cover the sclera (white of the eye). Because of this, there is physicall no way for a lens to gain access to the rear or either side of the eyeball. Phewf! #1. WEARING POORLY FITTED LENSES CAN DAMAGE YOUR CORNEA There is some truth to this one... Don't trust just anyone with your contact lens fitting! Your cornea is the part of the eye that reflects light. It is the transparent front part of the eye (the window) that covers the iris, pupil and anterior chamber. To prevent damage to the cornea, be sure to get regular eye check ups from your eye care professional to ensure you are wearing the best contact lenses for your eyes. We have many options and specifications that will guarantee your comfort and the safety of your vision. Breathe new life into your wardrobe with the season's freshest trends. Purchasing new frames can be overwhelming. But with a little guidance, the experience can be fun and exciting. Eyewear is a declaration of your personality and has the ability to introduce you to strangers without speaking a word. Eyewear has even become a signature staple for many celebrities. Think, Steve Jobs, John Lennon, Elvis. So where to begin when choosing new frames? Here are some suggestions to help you find your signature pair. Consider Your Script Starting off, we recommend you take your prescription strength into consideration. Not every script will look good in every frame. Our professional Opticians can immediately direct you away from any frames that aren't ideal for the lenses your prescription will require. For example if you're nearsighted with a strong, negative script, your lenses will be thicker. Thick lenses will look better in a smaller frame because the lenses get thicker as they spread out from the center. So a small frame will eliminate the thickest part of the lens. A large one would allow that bottle cap effect. Compliment Your Coloring. Skin tone plays an important part in finding the best frames to compliment your appearance. There are hundreds of skin tones but to simplify it; You have either a warm (yellow-based) or a cool (blue-based) skin tone. Here's a helpful trick: check out your veins. If they're more blue than green, you have a cool skin tone and should consider frames that are black, reddish brown, slate blue, or dark tortoise. Do your veins appear more green? That means you have a warm skin tone and will be best off in camel, khaki, or copper. For the outgoing warm, try a bold fire engine red. Contrast the Your Face Shape Pick frames that contrast your face shape, not ones that imitate it. An oval, symmetrical face shape is generally ideal but the percentage of people that possess that face shape is rare. Choosing frames that help us achieve this "oval effect" tend to compliment ones face shape the best. If a weak chin is problematic for you, a frame that's slightly wider at the bottom edge will give the lower portion of your face what your chin is lacking. If you have a circular round-face, try frames with sharp angles: rectangles, trapezoids, and the super trendy hexagonal frames will look awesome. Round glasses would accentuate fuller cheeks. If your cheeks and jowl expand further than your forehead, choose a frame with a dramatic top edge to avert eyes up. Check up the helpful chart below to identify frames suitable for your specific face shape. Be Yourself
Above all else, you do you! All of these suggestions are merely that... suggestions! Go with your gut. If you find a frame outside these guidelines that makes you feel good about yourself, break the "rules". There are hundreds of styles, shapes, color and brands when it comes to eyewear. This article aims to ease the process for you. But it won't work for every person, every time. Glasses are one of the first things people notice about us. What impression do you want to give off? It's your vibe. Own it with a pair that makes you feel fab, confident and mostly YOURSELF. |
AuthorAndrew Biondo, OD, FSLS is the Primary Medical Director at Kirkwood Eye Associates in Kirkwood, MO. Serving the greater St. Louis area, Dr. Biondo has 12 years of experience as an eye care provider, health educator & consultant to the specialty contact lens industry. His special interests include contact lenses, dry eye disease, glaucoma, macular degeneration, laser eye surgery & preventive vision care. Archives
October 2022
Categories |
Contact us:
|
Location:
|
Stay in the loop!
|










 RSS Feed
RSS Feed